How gut bacteria evade the immune system
New insight into how harmless gut bacteria avoid triggering inflammation
Researchers from the Max Planck Institute for Biology Tübingen address the long-standing question of how benign gut microbes evade the immune system. In doing so, they also reshape our understanding of how immune receptors interact with the bacterial motility protein flagellin. The scientists identified a new type of flagellin in the human gut, termed ‘silent flagellin’, that binds to the immune receptor Toll-like receptor 5 without inducing a pro-inflammatory response. The findings provide a mechanism for the immune system to tolerate beneficial microbes while remaining responsive to pathogens.

The human gut is the habitat of benign, beneficial, and sometimes harmful bacteria. In order to fight off these last-mentioned pathogens, the immune system first recognizes the presence of microbial products via various receptors. One of these is Toll-like receptor 5 (TLR5): it binds flagellin, the protein that makes up the bacterial flagellum, which bacteria use to swim. Once bound to flagellin, TLR5 induces a pro-inflammatory immune response. However, pathogens are not the only gut inhabitants producing flagellin; harmless and beneficial bacteria make it as well. This raises the question of how these beneficial bacteria evade the immune response. While some bacteria avoid TLR5 by producing flagellins that no longer bind the receptor, previous research showed that so-called commensal bacteria, which are harmless to their human hosts, produce flagellins with intact binding sites.
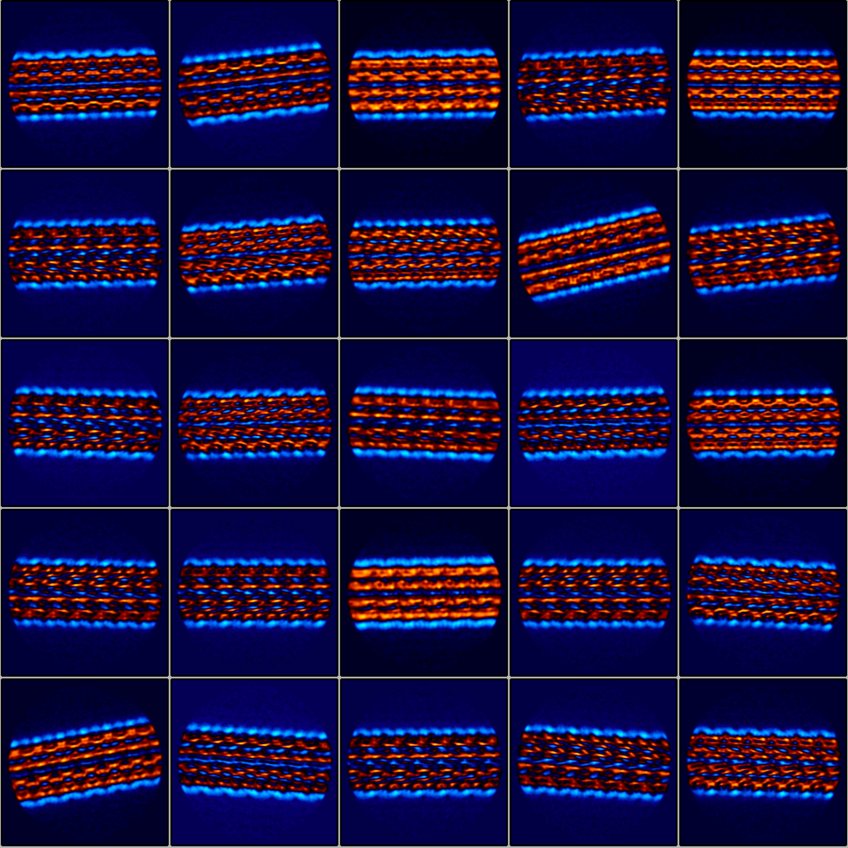
An international team led by researchers from the Max Planck Institute for Biology Tübingen now has an explanation. By screening 116 different flagellins for both TLR5 activation and binding, the researchers found that roughly half were unlike previously described flagellins. These flagellins showed strong binding to TLR5, similar to flagellins from pathogens, but failed to trigger an inflammatory response. Therefore, the scientists termed this new flagellin variant ‘silent flagellins’. Previously, flagellin binding to TLR5 was thought to be sufficient to activate the inflammatory response. The discovery that commensals produce flagellins that bind TLR5 without initiating an immune response challenges the prior understanding of how TLR5 is turned on.
Different ways of interaction
“We now know that bacterial flagellin can interact with TLR5 at least three in different ways: bind and induce an immune response, bind and not induce an immune response, and evade by not binding,” explains Ruth Ley, senior author of the study and director of the Department of Microbiome Science at the Max Planck Institute for Biology Tübingen. “It is remarkable how tunable the response of the TLR5 receptor is,” she adds.
Subsequent metagenomic analyses showed that silent flagellins are very common in the human gut and therefore represent “a substantial, previously unappreciated, yet physiologically relevant, population of TLR5 binding proteins,” says Sara Clasen, first author of the study. TLR5 is implicated in many gut-related diseases but also plays a role in other disorders such as cancer and neuropathy. The findings provide deeper insights into the mechanism of TLR5 activation and could therefore help better understand TLR5-related diseases.